Authors: Charlotte Davies, Sophie Windsor / Editors: Elizabeth Herrieven, Nikki Abela / Reviewer: Victoria Dulko / Codes: / Published: 08/01/2019 / Reviewed: 28/05/2024
Cardiac arrest in pregnancy is a potential presentation to the emergency department. If it happens, you are likely to be cognitively overloaded. Weve talked through what you need to do, then shared a checklist that specifies what you need to do, in the order you need to do it. Weve supported our blog with some awesome pictures by Sarah Payne and Jonathan Hurley. In real life, it is hoped many of these actions will happen simultaneously. But for it to work, you need to read it, and mentally rehearse it before you need it for real, as well as seeing what happens in your hospital.
This process is now termed resuscitative hysterotomy to reflect the potential benefits to the mother of performing the procedure, namely relieving aorto-caval compression, improving pulmonary mechanics and reducing oxygen demand. You may find it still referred to as a peri-mortem c-section in some resources. Recent evidence (Resuscitation 2025) suggests neonatal outcome is good – 45% survive.
Call for Help

This is mandatory, even if youre in the ED. Youre going to need a lot of handsnowand this is the quickest way to get them.
At our hospital, a maternal cardiac arrest bleep goes to the whole obstetric team, the midwife coordinator, the obstetric anaesthetist, the neonatal team and the medics, ensuring you are likely to get an obstetric member of the team to do the resuscitative hysterotomy and the neonatal team for the neonatal resus. If any of the team, e.g. neonates in a postnatal woman, are not required they can always leave.
Consider putting out an early major haemorrhage or code red call for some quick blood. Remember physiological signs of bleeding may not be present, and the physical presence of bleeding may not be evident it may be concealed.
If youre not the Consultant, consider calling them If its the middle of the night dont wait for them but theyd probably like to know and might need to provide some support to you and the team afterwards.
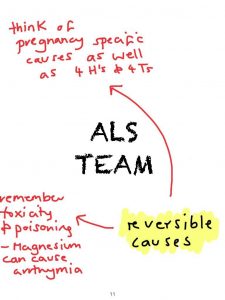
Advanced Life Support

Delivering advanced life support is going to be one of the initial components. Theres no changes to the algorithm. Give the drugs. Give the shocks. Youll need to allocate a team leader who is unlikely to be you, as if youre reading this, youre likely to be busy doing the hysterotomy. The team leader doesnt have to be a doctor it could be the paramedics who bring the patient in, an ALS trained Nurse, resus officer etc. In my department I would allocate an ACP if they were there.
Modifications to ALS for Pregnancy
Reduced venous return due to aortal compression from the foetus is not a cause of cardiac arrest, but wont help any resuscitation efforts, so it is worth reducing its effects. This can be minimised by uterine displacement pulling the uterus up and out of the pelvis first, then to the left, is considered better than pushing it. A left lateral tilt is no longer considered appropriate in cardiac arrest as then chest compressions arent effective. If the patient is peri-arrest, rather than in cardiac arrest, tilt the patient 15 degrees towards their left a wedge or blanket will be needed.
Then consider:
* Early intubation (preferably NOT with an LMA because risk of aspiration is much higher in pregnant patients). There is some narrowing of the airway in pregnancy, so you may need a slightly smaller tube.
* Slightly higher chest compressions – this is only one space higher – you don’t want to end up with clavicular compressions!
Prepare for Resuscitative Hysterotomy
This is applicable for patients more than 20 weeks (or suspected) gestation in cardiac arrest only any earlier than that and the foetus is unlikely to a) survive and b) have significant effects on the maternal circulation. If you think they are very pregnant, but dont have any confirmation, decide what you think is most appropriate. Youll be more likely to be cross with yourself for not doing it, than for doing it. The sooner the better. Theres no maximum duration of downtime now if its been 4 minutes or more with CPR, get the c-section done. If the patient isnt in cardiac arrest, but is just very poorly, get an obstetrician to help you ASAP.
Find the equipment in our cupboard its in a box in the resus cupboard. Where is it in yours? In reality, all you really need is a scalpel, and preferably some clamps. A thoracotomy tray will also have all you need.
Perform Resuscitative Hysterotomy
This YouTube video is well worth watching. It summarises everything we’re going to say or have said.
You dont have time for a gown/hat/mask or to wash your hands surgically but gloves and an apron will be very useful. Clean the skin then incise from the umbilicus to the pubic bone vertically. If youre used to doing horizontal (or Pfannenstiel) incisions, go for it. Try to avoid the urinary bladder which is close to the lower segment of the uterus. The bladder will probably be full, but dont waste time with a catheter. You might need some swabs to help you grip, and to control any bleeding count them in if possible. Those nice big surgical swabs will be easiest but if you cant find them, any sterile swabs will do.
After your incision, you should be able to spot the uterus, and deliver the foetus. Exposing, or delivering, the uterus is only done where there is bleeding from the broad ligament and in an arrest situation there shouldnt be much bleeding if there is, you would definitely need an obstetric consultant to assist.
After the baby has been delivered, dont forget the placenta! If the placenta wont come out easily, leave it in situ and wait for obstetric assistance it may be a placenta acreta, and pulling it out will make things worse!
Continue to resuscitate your patient and resuscitate the neonate too if applicable.
Correct Further Reversible Causes
Thromboembolism is the leading causes of death in pregnant women, and there is a reluctance to give thrombolysis. Case report numbers are small but if thrombolysis is indicated, it should be given, even after a resuscitative hysterotomy. Have a look at the MBRRAC report where they clearly state Neither pregnancy, caesarean section delivery or the immediate postpartum state are absolute contraindications to thrombolysis. Massive bleeding may result but there are case reports of good outcomes.
Debrief

We dont do this very often, so youre almost certainly going to need to organise a debrief. It can be useful to think about what youre going to say before youre suddenly leading a debrief. Maybe:
Thank you for attending this hot debrief. Thank you all for the work youve done.
Was there anything you felt we did particularly well as a team? Clinical care, teamwork, communication, leadership, other?
Was there anything you thought we could improve on?
Do you have any concerns?
I think a cold debrief is needed. Please write your email details on this sheet of paper, and we will be in touch to arrange a cold debrief.
Here’s a summary checklist – why not print it out, and stick it on top of your department’s emergency c-section kit, and then run a simulated peri-mortem c-section? If you prefer more pictures, there’s another checklist here. There’s a case written for you already! And if you’re feeling ready for a challenge, log in and take our SAQ on cardiac arrest in pregnancy!
There is also a link to a useful video from SMACC here.
Picture credits:
Sarah Payne, Jonathan Hurley
The latest @mbrrace report documents that the rate of Resuscitative Hysterotomy (aka PMCS) has more than doubled in the UK from 20 ? in 2017-19 to 43 ? in 2020-22. Newborn survival rates increased from 20% to 30%. pic.twitter.com/4vBmJ9emXl
Caroline Leech (@LeechCaroline) October 10, 2024
References
- Statement on Perimortem Caesarean Section from MOET. Advanced Life Support Group, 2016.
- Maternal Collapse in Pregnancy and the Puerperium (Green-top Guideline No. 56). Royal College of Obstetricians & Gynaecologists, 2019.
- Lippmann QK, Menefee SA. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. American Journal of Obstetrics & Gynecology, 2016.
- Carley S. Perimortem C-section at St Emlyn’s. St Emlyn’s, 2013.
- Chu JJ, Hinshaw K, et al. Perimortem caesarean section why, when and how. The Obstetrician & Gynaecologist. 2018; 20: 151158.