Author: Indy Karpha, Charlotte Davies, Heenal Raichura / Editor: Liz Herrievan / Codes: / Published: 09/12/2020
Suspected Venous thromboembolism (VTE) is a common presentation in the Emergency Department (ED), yet investigation and management of these conditions remains a challenge due to uncertainty regarding diagnostic tests, a spectrum in clinical presentation, and probably an element of defensive practice from a medico-legal perspective. Management of possible VTE is also a good example of the statistics that are so important to good rational medical care, and understanding of this is crucial in the Emergency Department. There are several key statistical methods that you must be aware of. Emergency Medicine trainees are often very clear on medical statistics, probably because the critical appraisal examination currently forms part of their exit exam. Make sure you can define sensitivity, specificity, likelihood ratios and pre-test probability our critical appraisal dictionary may help. If youre a RCEM member, wed suggest consolidating your knowledge with our short questions on specificity and sensitivity.
Whats all this got to do with VTE? Lets start by reminding ourselves about VTE Haematology Registrar Indy Karpha talks us through it.
Venous Thromboembolism
What exactly is VTE? A venous thromboembolism (VTE) is when a blood clot forms in a deep vein, commonly in the lower limbs or pelvis. This thrombus can embolise to the lungs, causing a blockage in the pulmonary arteries a pulmonary embolism (PE). The term VTE therefore includes both deep vein thrombosis (DVT) and PE.
When should it be suspected?
The commonest presentations encountered are lower limb DVT and PE.
DVT usually presents as a unilateral lower limb swelling with a hot, tender calf, pitting oedema, collateral superficial veins and possibly localised tenderness along the deep venous system. Typically the calf will be >3cm larger than the asymptomatic side. However, it is important to remember that a DVT may present with only one or a few of these features.
PE classically presents with shortness of breath and/or pleuritic chest pain. ABG may reveal a respiratory alkalosis due to hyperventilation, with a type 1 respiratory failure. The commonest ECG finding is a sinus tachycardia, but there may be a RBBB, R axis deviation, or the textbook description of S1Q3T3 (actually fairly uncommon). A chest x-ray should be performed to exclude any other significant pathology and to screen for potential indicators for the presence of a PE, such as a small pleural effusion or a new lung lesion.
Remember in patients with a history of malignancy, thrombophilia traits or intra-vascular access, VTE may present in more unusual places such as the upper limbs.
Risk Factors
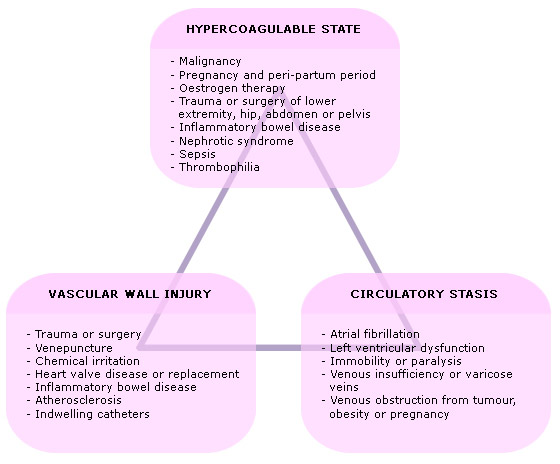
When VTE is a differential, it is useful to weigh up potential risk factors to support your diagnosis. Risk factors for a venous thromboembolism include:
We still do worry about long haul flights causing circulatory stasis but we should also ask about long-distance train/ car or coach journeys.
The Wells Score
The Wells score is also often used to weigh up the likelihood of VTE and in fact in some trusts is used as part of the vetting process for requesting radiology.
The Wells score, youll probably remember from medical school, is a series of questions on the clinical presentation and presence of risk factors for VTE. NICE guidance suggests that every patient with suspected VTE, after thorough clinical assessment, should have a documented Wells score. The score differs slightly between DVT and PE see below.
Suspected DVTwhat to do:
Do the DVT Wells score. The rest of the management is actually very dependent on this.
If the Wells score is unlikely (<2), get a D Dimer.
If the Wells score is unlikely and the D Dimer is negative, DVT can be effectively ruled out.
If the Wells score is unlikely and the D Dimer is positive, get a doppler US of the lower limb. This can be done without anticoagulation if the doppler will happen within 4 hours of being requested. Otherwise, the patient should receive a shot of parenteral anticoagulation, normally a low molecular weight heparin like enoxaparin or dalteparin (consult your trust policy).
If the Wells score is likely, get a doppler within 4 hours of requesting, or anticoagulate and organise a doppler US if it cant be done within 4 hours.
According to NICE guidance, you still need to get a D Dimer because if the patient has a positive D Dimer AND the proximal doppler is negative, you need a repeat scan to rule out proximal extension of a superficial/distal thrombus which may present later. However, NICE guidelines refer to proximal leg vein ultrasound scans throughout their guidelines. Most hospital trusts perform entire leg scans (proximal and distal leg vein ultrasound scans). Therefore, in most Trusts, a repeat leg Doppler would not be required as the distal veins would have already been scanned to look for a thrombus (and so there would be no ongoing concern of proximal extension of a potential clot).
If the D Dimer is negative AND the doppler negative, DVT can be ruled out.
If the D Dimer is positive AND the doppler is positivethey have a DVT! Continue LMWH and organise longer term anticoagulation, such as a vitamin K antagonist (e.g. warfarin) or DOAC (e.g. apixaban)

The process is similar for PE, but the Wells score slightly is different.
So, if you think your patient has a PE
First risk stratify your patient by doing the Wells score.
If it is likely (>4 points), no need for D Dimer. Instead get imaging either immediately, or anticoagulate whilst you await this. The NICE guidance is suggestive of CTPA as better than VQ, but service provision is likely to differ from trust to trust.
If the Wells score is unlikely (4 points), get a D Dimer (Note that the score is different for PE compared to DVT).
If the Wells score is unlikely and the D Dimer negative, PE is unlikely here.
If the Wells score is unlikely and the D Dimer positive, organise immediate imaging or anticoagulate whilst you wait.
NB If your CTPA is negative but you suspected both DVT and PE, it might be worthwhile getting a doppler US of the leg as well.

The PERC rule may also be useful but as this is only valid in low risk patients, you need to risk stratify your patient (i.e. calculate a PE wells score) first. For more details, please look here, or have a look at the original paper here.

Ambulatory Care?
As a large proportion of patients are likely to require Doppler US for suspected DVT, more and more trusts are now offering an ambulatory DVT service, in which the patient receives a parenteral anticoagulant, is discharged from the hospital and returns for a doppler US the next day. This prevents unnecessary inpatient stays whilst awaiting scans.
Not all patients are safe to go home BTS and NICE guidelines have different suggestions which weve interpreted and summarised below.
DVT: Admit if whole leg DVT, systemically unwell, non ambulatory patient.
PE: Admit if systemically unwell

The Statistics
So, why is this what we do?
This is where all those statistics come into play. What you do, depends on how likely you think it is that this patient has VTE. Its easy to tie yourself in knots, but if you remember the basic statistics, everything makes sense. Ideally, we want a test with 100% sensitivity and 100% specificity so it finds all the DVTs without missing any, but doesnt identify a non-existent DVT. The only test that does this is almost certainly a post mortem examination, and even that Id doubt is 100% so our next best test is a duplex scan. So why dont we duplex scan everyone? Resources come in to play but if you extrapolate this to ?PE a CTPA for everyone is a huge amount of radiation and contrast, before you even consider the availability. Theres also an argument that the more you do, the more patients expect you to do, and the more often they return but thats probably not appropriate for now.
The process above has some key points:

Suspected DVT / PE in Pregnancy
If DVT or PE is suspected in pregnancy, investigation with imaging is first line. D-Dimer is unreliable in pregnancy, as it is usually elevated in pregnancy anyway. The pre-test probability is already high, as pregnancy is a VTE risk factor, that despite the DiPEP study, and the YEARS criteria for pregnancy, investigation with imaging is your first line.
If suspected DVT, most hospital trusts will arrange a unilateral lower limb Doppler ultrasound scan.
If suspected PE, bloods, ECG, Chest x-ray (+/-ABG) should be performed to consider and exclude alternative diagnoses. Thereafter, bilateral lower limb ultrasounds can be arranged to screen for DVT (and if positive, potentially extrapolate for the presence of PE). If the bilateral lower limb scans are negative, CTPA (low-dose radiation) or VQ scan is considered.
Unprovoked VTE
Anyone aged >40 with UNPROVOKED VTE (ie, no risk factors), should have the following checked:
- Full clinical history with systemic enquiry to screen for red flag symptoms (including constitutional symptoms and gynaecological history in female patients)
- Clinical examination including abdominal examination to screen for any intra-abdominal or pelvic masses contributing to DVT
- Bone profile, Liver function tests and PSA (in male patients): to detect hypercalcaemia, deranged LFTs and elevated PSA levels as potential red flag indicators of malignancy
- Urine dip: to screen for microscopic haematuria as a potential red flag indicator of malignancy
- Breast Exam (+/- mammogram) in female patients: to screen for any abnormal lumps or changes
- Consider Chest x-ray in patients with confirmed DVT and a significant smoking history
- Until March 2020, 2-week-wait CT Abdomen / Pelvis +/- Chest was advised to screen for malignancy as a potential contributing cause for VTE. However, new NICE guidelines (NICE Guideline NG158; 1.8, March 2020) advise that CT imaging should be reserved for those patients with any red flag symptoms or signs. As a result, some trusts are opting to screen for malignancy with the above measures as well as Chest x-ray and US Abdomen / Pelvis (to allow for basic imaging / screening for malignancy).
Thrombophilia Screening
This is often considered in patients presenting with recurrent unprovoked VTE or with a strong family history of VTE. However, in general it is rare that this should be investigated in the acute setting.
Essentially, the only alteration in management if there was an underlying thrombophilic state, would be with regard to duration of anticoagulation. So, in patients with unprovoked VTE, or with a first degree relative who has also had an unprovoked VTE, thrombophilia screening can be considered at the stage when anticoagulation is to be stopped.
Other points to consider
There are a number of other issues to bear in mind when assessing patients with VTE.
- Patients with confirmed DVT should be offered below knee graduated stockings (affected leg only) about a week after diagnosis or when swelling has reduced sufficiently (in the absence of contraindications).
- TEDS should be worn on the affected leg for 2 years post DVT (get them changed 2-3 times a year).
- Heparin is an animal based product (porcine) and patients should be advised of this, as some patients may have concerns or religious beliefs which can impact management.
The D Dimer
The D-dimer should only be checked in patients with suspected DVT or PE after a clinical history and examination have been performed. If the suspicion of DVT or PE remains, then a D-dimer test should be performed. In the mean-time, a Wells score can be calculated. If the Wells score is <2 (unlikely DVT), then the D-dimer result can be reviewed to aid the decision of the next steps.
The D-Dimer is essentially a marker of fibrin breakdown, and as such is used to aid diagnosis of VTE, as well as a marker of DIC. However, there is a high rate of false positive as it can be elevated in several other conditions, including:
- Infection (including COVID)
- Pregnancy
- DIC
- GI haemorrhage
- Cancer
- AF
- Trauma
- Smoking
- Age
- And the list continues..!
It should also be remembered that VTE CAN occur in the presence of a negative D Dimer, so the whole clinical picture needs to be taken into account when assessing these patients.
Direct Oral Anticoagulants (DOACS)
I thought it would be worthwhile briefly thinking about the use of DOACS in VTE. The benefits of the DOACS is that the onset of therapeutic activity is quick (within a few hours), there is no drug level monitoring required, and the half life is fairly short, so effects stop rapidly after stopping treatment.
Examples of commonly used DOACs include Rivaroxaban and Apixaban. These are Factor Xa-inhibitors. At present there is no antidote (like octaplex for warfarin). This raises issues with regard to reversal in the presence of bleeding. Moreover, it should be remembered that Rivaroxoban should not be offered in patients with renal impairment, potential for drug interactions, or deranged LFTs. It does however offer a more convenient alternative than warfarin for longer-term anticoagulation.
In Summary
VTE is common in the ED and proper investigation is needed for diagnosis. Always calculate the Wells score and measure a d-Dimer if indicated, but dont forget to take the clinical picture into consideration when managing these patients.
Further Reading
- Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000 Mar;83(3):416-20.
- Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003 Sep 25;349(13):1227-35.
- Dunn JS, Kendall JM. Deep Vein Thrombosis in the ED. RCEMLearning, updated: 2024.
- Crane S, et al. Pulmonary Embolism. RCEMLearning, updated: 2023.

