Author: Ashleigh Lawrence Ball / Questions: Chris Connolly / Codes: / Published: 06/02/2018
It’s 5am, the pre-alert phone rings. The ambulance service are bringing in a patient with acute difficulty in breathing. From the observations you’re given, the patient sounds sick. ETA: 5 minutes. What goes through your mind?
Acute shortness of breath can be due to number of causes – are the lungs full of fluid or thick infected phlegm? Is there life-threatening bronchospasm? Do you need to call ITU or can this patient be managed in a ward-based environment? Let’s consider a general approach to shortness of breath in the ED and then the specific management of two of the commonest causes of acute dyspnoea COPD and acute asthma.
A General Approach
Difficulty in breathing is a non-specific symptom, and although we tend to immediately blame the lungs, there is a myriad of non-respiratory causes to consider. A good history and examination will help you to elucidate the cause – often easier said than done when the patient is in resus in extremis!
It’s an old trope by now, but it works – start the assessment of all sick patients with an evaluation of the ABCDEs. This helps prevent bias from tunnelled vision – a problem can cause the perception of shortness of breath but may only be fixed by treating the underlying cause – for example, a partial airway obstruction may result in shallow breaths and use of accessory respiratory muscles or diabetic ketoacidosis will cause Kussmaul’s respirations in order to compensate for the metabolic acidosis.
Oxygen
A venturi mask is often the best way of doing this – our oxygen blog, and the BTS oxygen guidelines (which we have gone over in a podcast) give you some tips on how to do this. Remember, hypoxia kills before hypercapnia. Do not be reluctant to put oxygen on – you can always turn it down once you’ve got some more information, but be aware that the oxygen may be the culprit if they start becoming drowsy.
Oxygen saturation monitoring will give you an idea of oxygenation but will not tell you about ventilation. An arterial blood gas may just change what you’re going to do. Review the results carefully before labelling any changes as “chronic” – we’ve all been caught out, and any significant acidosis will be new.
Fluids
Be judicious with fluid – acute pulmonary oedema may be the cause of the dyspnoea. Conversely, sepsis or metabolic derangement can result in tachypnoea – this may need large amount of fluid to stabilize the patient. Overload can occur, even in patients with previously normal LV function and may just make treating the patient that little more complicated. Make a careful assessment of the patient’s fluid balance status and if you’re not sure, give small but effective boluses and review the response.
Consider antibiotics in all patients with a cough or fever presenting with shortness of breath but remember that severe sepsis from any source (not just pneumonia) can cause difficulty in breathing and an oxygen requirement.
If your patient is tiring, or not oxygenating or ventilating adequately despite aggressive resuscitation, it is probably time to call your intensive care colleagues to consider invasive and non-invasive ventilation strategies (covered here).
We’re now going to talk in a bit more detail about some of the more common causes of shortness of breath.
COPD
NICE define an exacerbation of COPD as “a sustained worsening of the patient’s symptoms from their usual stable state which is beyond normal day to day variation and acute in onset”.
We see many patients who attend the emergency department with an exacerbation of their COPD. They normally present with a worsening cough, shortness of breath, increased sputum production or a change in sputum colour. On examination, they are often wheezy, but may have areas of reduced air entry due to gas trapping or bullae. Arterial blood gas sampling may show hypoxia with or without hypercapnia.
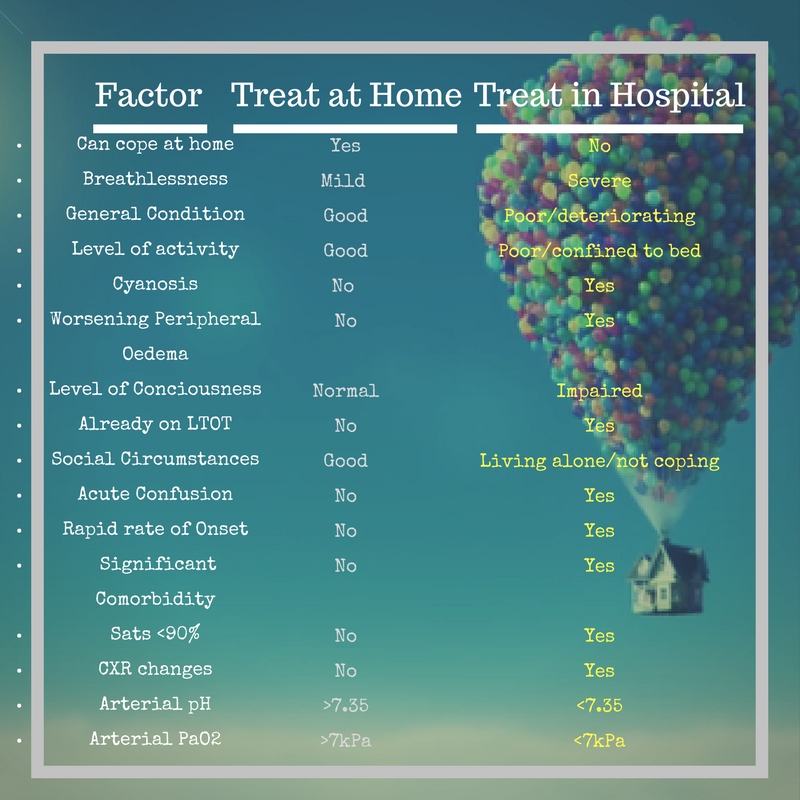
The majority of these patients can be managed with simple measures. Standard medical treatment for these patients is controlled oxygen to maintain saturations between 88-92%, nebulised salbutamol 2.5-5mg and ipratropium 500mcg (driven with air rather than oxygen), prednisolone 30mg and antibiotics if they report that their sputum is more purulent, or you suspect pneumonia. NICE has clear suggestions for when people can be treated at home with their exacerbation:
If oxygen is required to maintain an SpO2 of 88-92%, you can use nasal cannulae underneath the nebuliser mask. Nebulisers requires flow rate of 6-8l/minute, which may be too much oxygen in a subset of patients.
Non invasive ventilation (NIV) should be considered within 60 minutes of arrival to hospital in all patients with an exacerbation of COPD and a persistent respiratory acidosis (pH <7.35 and PaCO2 >6 kPa) in whom medical treatment is unsuccessful. Many hospitals would require you to speak to a senior before commencing this. Repeat your arterial blood gas an hour after starting NIV, to see how treatment is helping. Patients with COPD need bilevel positive airways pressure (BIPAP) so you need to set the expiratory positive airway pressure (EPAP) and inspiratory positive airway pressure (IPAP). The British Thoracic Society recommend a starting EPAP of 3cmH20 and IPAP of 15 if the pH <7.25.
Some patients will need a direct referral to ITU for consideration of intubation and mechanical ventilation. These patients are often very acidotic, very hypercapnoeic and too obtunded to protect their airway during NIV or too agitated to tolerate the tight fitting facemask required for effective treatment. You should also consider asking ITU to review any patient with a pH of <7.26 as studies suggest they have a high failure rate for NIV and require earlier mechanical ventilation.
All patients starting on NIV should have a clear escalation plan documented in case they continue to deteriorate.
Acute Asthma
CXR = only if suspect pneumomediastinum, pneumothorax, consolidation, life threatening exacerbation, ventilation requirement, or failure to respond to treatment.
Finally
Don’t forget to take a breath yourself! Patients presenting with shortness of breath will be anxious and their anxiety makes their shortness of breath worse. If you stay calm, they’ll relax (at least a little) and you’ll give yourself time to think. The first steps are always the same – give high flow oxygen and assess the ABCDEs. Stabilise the patient and then you can worry about the rest.
Further Reading: