Author: Olajide Kamal Badmus, Riad Hosein / Editor: Lauren Fraser / Codes: / Published: 02/09/2021 / Reviewed: 21/11/2024
*This work is dedicated to Riad Hoseins wife, Najma Mirza, who sadly passed away after a short illness. She gave him the idea of the module over dinner.
Context
Wounds are common presentations to the emergency department (ED). As such, we aim to guide ED Practitioners towards making an adequate assessment and appropriate management of acute wound presentation in our ED.
This session focuses on improving our skills and knowledge of wound management in an ED setting. It emphasized proper wound classification, physiology of wound healing, and the surgical skill set needed in the emergency management of wounds.
Definitions
A wound is a break in the skin’s epithelial integrity with disruption of possibly deeper tissues, including dermis, fascia, muscle, and bone.10
Anatomy of the Human Skin

A wound can also be characterized in its complexity as this incorporates useful clinical information with implications for management.
A simple wound involves the skin and subcutaneous tissue, without significant tissue loss and any associated complications.
A Complex wound is associated with significant tissue loss or devitalization; communicates with viscera (e.g. fistula), body cavities (e.g. laparostomy), joints or prosthesis; or has associated injuries or paths leading to vital structures.
A complicated wound has suffered a secondary complication such as an infection, ischemia (flap necrosis), hematoma, or compartment syndrome.6
Clean
- An uninfected operative wound in which no inflammation is encountered and no systemic tracts entered (respiratory, alimentary)
- Closed by primary intention and are usually not drained
Clean, contaminated
- An operative wound in which systemic tract(s) are entered under controlled conditions and without contamination
Contaminated
- Includes:
- Open traumatic wounds (open fractures, penetrating wounds)
- Operative procedures involving:
- Spillage from the GI, GU or biliary tracts
- A break in aseptic technique (open cardiac massage).
- Microorganisms multiply so rapidly that a contaminated wound can become infected within 6 hours.
Dirty/Infected
- Heavily contaminated/infected wound before an operation
- Includes:
- Perforated viscera
- Abscesses
- Wounds with undetected foreign body/necrotic tissue.1
Most wounds are usually easy to manage and result in desirable secondary outcome if appropriate steps are taken during contact with medical care.
Learning Bite:
Most ED presentation will fall within the clean-contaminated or contaminated wound classification. While clean-contaminated wounds can be closed by primary intention, contaminated and dirty wounds will be referred to the appropriate speciality for irrigation, debridement and formal closure in theatre.
Phases of wound healing
The wound healing process comprises several phases that take days to years to achieve almost initial skin integrity. A wound usually heals by one of primary, secondary, or delayed secondary intention.
Phases of wound healing

In the event of a tissue injury, the body initiates a cascade of overlapping cellular and extracellular activities that immediately start post-injury and lasts several months. This process comprises four distinct yet overlapping phases.
Haemostasis:
- Starts immediately following injury.
- Activation of the coagulation cascade and temporary constriction of blood vessels directly supplying the injured area.
- The platelets trapped in the blood clots kick starts a series of inflammatory response.
Inflammation:
- Activation of the complement cascade within 1-2 days of the injury.
- Wound infiltration by polymorphonuclear leukocytes. (PML)
- PML occupies the wound sites, phagocytose bacteria, and other foreign particles, kill them off and goes dormant.
- During this period, epithelial cells from both edges start depositing the basement membrane as they migrate towards each other.
- Macrophages activation in 48-72hrs and act as the regulatory cells for repair by producing growth factors responsible for the proliferation.
Proliferation:
- Starts about day three and last 2-4 weeks.
- Characterized by fibroblast migration and deposition of the extracellular matrix.
- Fibrin matrix is subsequently replaced by newly formed granulation tissue.
- Epithelization continues
Remodelling and scar maturation:
- May continue for several months.
- Continuous breakdown of collagen and remodelling of the extracellular matrix.
- Decrease in underlying contractile connective tissue brings the wound edges closer.
- Collagen bundles increase in diameter as well as increasing the tensile strength of the wound.
- Vascularity decreases and surface scar appear paler.

Learning Bite
Following scar maturation, the skin collagen fibre only regains a maximum of 80% of its pre-injury strength and integrity. 2
Types of Wound healing
Primary Intention:
- Occurs in simple non-complicated wounds, when it is closed within 12-24hrs of its creation.
- Due to minimal disruption to the surrounding connective tissue and epithelial basement membrane, epithelization predominates over fibrosis.
- There is usually a balance between all phases of the healing process.
- There is a direct approximation of the wound edges, leading to rapid wound healing and good cosmetic outcome.
Delayed Primary Healing:
Also known as healing by tertiary intention.
- Usually found in poorly outlined, or contaminated wound.
- Due to the risk of infection, wounds are left open to allow appropriate host response and the inflammatory process destroys the contaminating bacteria before closure.
- Wound are debrided and left open with gauze packing or stay sutures.
- The wound is then revisited for closure or allowed to heal by secondary intention if an infection is evident.
- The wound mostly retains its tensile strength since the collagen metabolism is usually unaffected.
Note: Both forms of primary closure allow synchronous healing of superficial and deep parts to occur in unison.
Secondary Intention:
- Occurs in complex and traumatic wounds.
- There is usually extensive skin and surrounding structure disruption.
- Due to the wound margins insufficient appropriation, there is the recruitment of extracellular matrix and laying down of collagen fibres with loss of tensile strength.
- Time of recovery is more prolonged than primary healing.
- There is usually associated wound contractures and functional restrictions.
Factors influencing tissue healing
Local Factors:
- Devitalized tissue
- Clot
- Foreign Bodies
- Infection
- Tissue hypoxia
- Acute Vascular damage or tight sutures
- Chronic
- Diabetic microvascular disease
- Atherosclerosis
- Venous Hypertension
Systemic factors:
- Nutritional deficiency Vitamin A, C, protein and zinc
- Drug treatment: glucocorticoids and cytotoxic drugs
- Diabetes
- Body irradiation
- Hypercatabolic states
- Neoplasia, Jaundice, Uremia, Burns

Principal steps in the management of an acute wound
| Steps | Core issues and activities |
| Assessment |
Accurate history: the magnitude of trauma, contamination.
Diagnosis and stratification Associated injuries: neurovascular, musculoskeletal, visceral Need for referral/multidisciplinary approach/triage |
| Preparation |
Patient Consent
Prophylaxis antibiotic tetanus(if required) Analgesia/anaesthesia/sedation and associated monitoring if required |
| Patient | Cooperative patient |
| Kit |
Suture pack
Needle holder Tissue forceps tooth and non-tooth Scissors Swabs Saline Antiseptic solution Sutures appropriate GlovesGood lighting Good magnification PPE as required Appropriate height of the bed |
| Staff |
Let nurses know about management plans.
Let the ED physician in charge (EPIC) know about the management plans |
| Definitive treatment |
Exploration
Irrigation Debridement Haemostasis Closure: when, how, where, which first? Drainage Referral/multidisciplinary approach |
| After-care |
Dressings
Removal of sutures/splints Wound care advice Surveillance for complications Physiotherapy and rehabilitation |
HISTORY
Timing and mechanism of injury are essential
- Crush injury is more likely to destroy the blood supply
- Contamination of wound by a foreign body increases the likelihood of infection
- Bite wound poses risks of blood-borne diseases and needs to be thoroughly assessed with appropriate cover where necessary.
- Associated injuries in other regions may complicate management protocols.
Associated past medical histories such as diabetes and peripheral vascular disease, anticoagulant use, Immunization history, social history such as smoking and occupational history may predict healing.
-Consider self-harm and safeguarding concerns in the elderly, the pediatric or patient with a mental health history.
EXAMINATION
General body examination.
Inspection of the wound site.
- Assess depth but avoid the temptation to probe deeper (if it cannot be reliably determined, get more specialist help)
- Prescence of a foreign body.
- Assess the distal neurovascular bundles
- Check for underlying bony injury.
RELEVANT INVESTIGATIONS
X-ray is highly sensitive for detecting radiopaque foreign body. Ultrasound has high specificity but moderate sensitive for detecting foreign body. However, the sensitivity for radiolucent objects is almost 97%.7 CT scan may be required in selected cases.
NEED FOR REFERRAL
A wound to select areas
E.g., Burns, significant face or hand injuries and others.
PROPHYLAXIS
- Tetanus immunization and prophylaxis following injuries.
A decision regarding tetanus prophylaxis must be made in every patient with an injury.
| Immunization status | Immediate Treatment | Later Treatment | ||||
|---|---|---|---|---|---|---|
| Clean wound | Tetanus prone | High-risk tetanus prone | ||||
| Those aged 11 years and over have received an adequate priming course of tetanus vaccine with the last dose within 10 years. | None required | None required | None required | Further doses as required to complete the recommended schedule (to ensure future immunity) | ||
| Children aged 5-10 years who have received priming course and preschool booster. | ||||||
| Children under 5 years who have received an adequate priming course. | ||||||
| Received adequate priming course of tetanus vaccine but last dose more than 10 years. | None required | Immediate reinforcing dose of vaccine | Immediate reinforcing dose of vaccine | One dose of human tetanus immunoglobulin in a different site | ||
| Children aged 5-10 years who have received priming course but no preschool booster. | ||||||
| Includes UK born after 1961 with history of accepting vaccination. | ||||||
| Not Received adequate priming course of tetanus vaccine (includes uncertain immunization status and born before 1961) | Immediate reinforcing dose of vaccine | Immediate reinforcing dose of vaccine | One dose of human tetanus immunoglobulin in a different site | Immediate reinforcing dose of vaccine | One dose of human tetanus immunoglobulin in a different site | |
Adapted from post exposure management for tetanus prone wounds.4,5
- Prophylactic Antibiotic
Routine antibiotic prophylaxis for simple wounds has no scientific basis. However, following good history taking and proper assessment of individual wounds,
Prophylactic antibiotics may be prescribed for some select patient group. Examples include;
Risk Factors for wound infection
- Location: leg and thigh, then arms, then feet, then chest, back, then face then scalp
- Contamination with devitalized tissue, foreign matter, saliva, stool
- Blunt (crush) mechanism
- Presence of subcutaneous sutures
- Types of repair: risk greater with sutures > staples > steri-strip
- Anaesthesia with epinephrine
- High-velocity missile injuries
- Diabetes.
Adapted from Risk Factors for wound infection.9
- Analgesia/Anesthesia
- Local anesthesia to the injury site serves both functions of allowing for reasonable wound exploration and pain and anxiety control.
- Lidocaine (Xylocaine) is the most common agent used for local and regional anaesthesia. It is safe and fast-acting.
- Dosage: 1 % Lidocaine =10mg/ml 3mg/kg without adrenaline. 7mg/kg with adrenaline. (Used to prolong the anaesthetic effect of Lidocaine but at the risk end artery vasospasm and subsequent tissue ischemia). It should be avoided in end organs such eyes, ears, nose, fingers, toes and the penis.
- Reversal agents for vasospasm induced Lidocaine with adrenaline include; subcutaneous phentolamine or topical nitroglycerine.9
- Local anaesthetic toxicity is uncommon but can carry a significant mobidity or mortality.
- Manifestations of local anesthetic toxicity can appear 1 to 5 minutes after the injection, but onset may range from a few seconds to as long as 60 minutes.
Toxicity manifestations can be categorized as follows:
– CNS manifestations: Systemic toxicity initiates with symptoms of CNS excitement such as the following: Circumoral and/or tongue numbness, metallic taste, lightheadedness, dizziness, visual and auditory disturbances (difficulty focusing and tinnitus), disorientation, drowsiness, this may be followed by a rapid CNS depression, muscle twitching, seizures and coma.
– Respiratory depression and arrest.
– Cardiovascular manifestations: Chest pain, Shortness of breath, Palpitations, Diaphoresis, hypotension and syncope.
In lidocaine toxicity management, intravenous lipid emulsion (Intralipid) is the drug of choice.
Learning Bites
Adrenaline prolongs the anaesthetic effect of Lidocaine but at the risk of delay wound healing and lower resistance to infection.
4. Exploration
Wound irrigation and adequate toileting to flush out dirt particles with warm saline (0.9%sodium chloride). It also helps assess anatomical extents of injuries and determine any associated injuries to underlying structures.6 Debridement and closure may be done in a well-controlled setting if indicated.
Definitive Treatment:
- Closure
Immediate closure to allow healing by primary intention
Delayed closure followed by healing by delayed primary intention.
Healing by secondary intention.
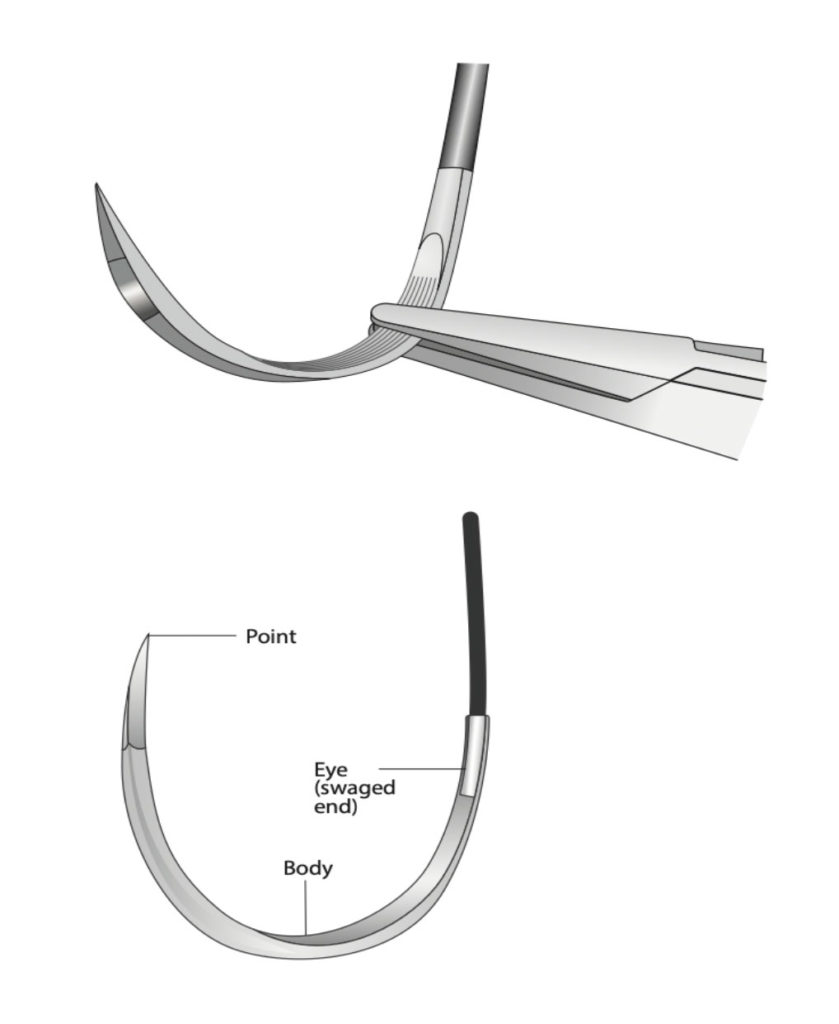
Needle types
Some of the instruments (with descriptions) used for closing wounds include: Needle
The main types of needle include:
- Tapered
- Gradually taper to the point and cross-section reveals a round, smooth shaft.
- They are used for easy to tear internal tissues like bowel or blood vessels or can be used to close fascia as part of a two-layer closure.
- Cutting
- Triangular tip with the apex forming a cutting surface.
- Used for tough tissue, such as skin (use of a tapered needle with skin causes excess trauma because of difficulty in penetration).
- Reverse cutting needle
- Similar to a conventional cutting needle except for the cutting-edge face down instead of up. This may decrease the likelihood of sutures pulling through soft tissue.
- Double ended needles are used when anastomosing vessels. They are occasionally seen in your thoracotomy trays and are very useful with pledgets to repair the ventricular wounds.

Suture materials
Most sutures with the suture material swaged onto the base of the needle
Shapes vary from a quarter circle to five-eighths of a circle, depending on how confined the operating field is
Choice of the needle should ‘alter the tissue to be sutured as little as possible’ and is dependent on:
- The tissue being sutured (when in doubt about the selection of a tapered point or cutting needle, choose the taper for everything except skin sutures)
- Ease of access to the Individual tissue preference.
Properties of suture material
- Handling of a suture
- Memory
- The tendency to stay in one position
- Leads to difficulty in tying sutures and knot unravelling
- Elasticity
- Knot strength
- The force required for a knot to slip
- Important to consider when ligating arteries
- Memory
- Tensile strength
- The force necessary to break a suture
- Important to consider in areas of tension (linea alba)
- Tissue reaction
- Undesirable since inflammation worsens the scar
- Maximal between Day 3&7
Types of sutures
- Monofilament (Ethilon or Prolene)
- Consists of a single smooth strand
- Less traumatic since they glide through tissues with less friction
- May be associated with lower rates of infection.
- More likely to slip and should be secured with 5 or 6 ‘throws’ (in contrast to 3 throws with multifilament)
- Preferred for skin closure because they provide a better cosmetic result
- Multifilament (Mersilk or Mersilene)
- Consists of multiple fibres woven together
- Easier to handle and tie and knots are less likely to slip.
Classification of sutures
Non-absorbable suture material
Composed of materials which can be:
- Naturally occurring (Mersilk, cotton and steel)
- Synthetic (Prolene, Ethilon)
Absorbable suture material
Composed of biodegradable materials which can be?
- Naturally occurring (degraded enzymatically)
- Catgut (no longer used in routine practice)
- Consists of processed collagen from animal intestines
- Broken down after seven days
- Chromic catgut
- Consists of intestinal collagen treated with chromium
- Loses tensile strength after 2-3 weeks and is broken down after three months
- Synthetic
- Degraded non-enzymatically by hydrolysis when water penetrates the suture filaments and attacks the polymer chain
- Tend to evoke less tissue reaction than those occurring naturally.

Whats on the packaging:

Suture pack contents
- Needle holder
- Forceps
- Scissors
- Scalpel
- Gauze
Add on includes:
- Appropriate Suture size
- Saline++++
- Betadine/ povidone/ alcohol/ chlorhexidine
- LA- Avoid with adrenaline, safe dose of Lignocaine = 3 mg/kg (1% = 10 mg/ml)
- Hypodermic Needles/ Syringe
Suture pack:
Scissors
Forceps
Needle holder
Blades
Use of blades
Learning Bite:
Use LA (avoid using adrenaline in end organs/ digits) before cleaning wounds. Do not inject in infected or inflamed tissues.
Exposure
Good Lighting
Magnification
Adequate Positioning
Suturing Techniques
Mounting of the needle
1.Simple interrupted sutures
This can be either:
- Simple Interrupted
- Used on majority of wounds
- Each stitch is independent
NEEDLE INSERTION
INSTRUMENT TYING

2. Vertical vs Horizontal Mattress sutures
VERTICAL MATTRESS
HORIZONTAL MATTRESS

Vertical Mattress – Useful for everting skin edges “Far-far-near-near”

Horizontal Mattress – Useful for single-layer closure of lacerations under tension

3. V-shaped wound closure

How do you Hand tie?
HAND TYING FIRST THROW FIRST KNOT
HAND TYING SECOND THROW FIRST KNOT
HAND TYING SECOND KNOT
KNOT COMPLETION
This is done by alternating between the first and second knots
HAND TYING WITH SUTURE
Aftercare
Dressings/ Surveillance for complications
- Consider splinting digits, joint surfaces
- Check tetanus status
- Pre-printed wound care instructions
- Pt must understand signs of infection
Once the scab has fallen off, massage and moisturize to reduce the risk of keloids and hypertrophic scar formation, this includes avoiding sun exposure, sunblock.
The district nurse or GP can follow simple, uncomplicated wounds for further wound care and suture removal.
Higher risk wounds must be reviewed earlier (24-48hrs), either at the ED clinic or respective speciality. Examples of high-risk injuries: hand wounds, Bites, heavily contaminated or wounds requiring antibiotics.
REMOVAL OF SUTURES
| Anatomic Area | Days until Removal | External suture size | Buried Absorbable suture size |
| Face | 4-5 | 5-0 or 6-0 | 5-0 |
| Scalp | 10-14 | 4-0, staples | 3-0 |
| Upper body | 7-10 | 4-0 | 4-0 |
| Hand | 7-10 | 4-0 or 5-0 | 4-0 |
| Lower body | 10-14 | 4-0 | 3-0 |
| Over joint (splint recommended) | 14-21 | 4-0 | 3-0 |
Adapted from Face and scalp lacerations: timing for suture removal.10
- Physiotherapy and rehabilitation
- Injuries with associated fracture
- Injuries affecting joints
- Injuries to special areas.
- Badawy A. Basic surgical skills final. Slideshare, 2016.
- Enoch S, Leaper DJ. Basic science of wound healing. Surgery Oxford International Edition, Volume 26, Issue 2, 31 37, 2008.
- Cave G, Harrop-Griffiths W, Harvey M, et al. (n.d.). Management of severe local anaesthetic toxicity. Association of Anaesthetists, 2010.
- Health England, P. (2019a). Post exposure management for Tetanus Prone Wounds.
- Health England, P. (2019b). Tetanus-prone wounds* Puncture-type injuries acquired in a contaminated environment and likely therefore to contain tetanus spores* e.g. gardening injuries Wounds containing foreign bodies* Compound fractures Wounds or burns with systemic sepsis Certain animal bites and scratches**.
- Kumar S, Leaper DJ. Classification and management of acute wounds. Surgery (Oxford), 23(2), 4751, 2005.
- Mankowitz SL. Laceration Management. Journal of Emergency Medicine, 53(3), 369382, 2017.
- Parrish WR, Roides B. Physiology of Blood Components in Wound Healing: an Appreciation of Cellular Co-Operativity in Platelet Rich Plasma Action. J Exerc Sports Orthop 4(2):1-14, 2017.
- Simon BC, Hern HG. Wound Management Principles. ClinicalKey. Rosens Emergency Medicine: Concepts and Clinical Practice. 2018; Chapter 52.
- Usatine RP, Coates WC. Laceration and Incision Repair. ClinicalKey. Pfenninger and Fowlers Procedures for Primary Care, 2020; Chapter 19.
Additional Resources
Courtesy of QEHB Audio-visual department
