Author: Sarah Stobbs / Editor: Janet Skinner / Reviewer: Joe Schrieber, Caitriona Considine / Codes: CC10, CC5 / Published: 09/03/2020
Context
Alcohol abuse is undoubtedly a huge social problem in the UK. It is responsible for many unnecessary attendances to Emergency departments (ED) and is an enormous burden on the NHS, which must treat the complications of alcohol abuse. The Royal College of Physicians advise weekly alcohol limit of 21 units for men and 14 units for women.1
The Scottish Health Survey 2017 found 16% of adults were drinking to hazardous proportions using the alcohol use disorder identification test (AUDIT) published by the World Health Organisation.2
Since 2012 the number of alcohol-specific deaths in Scotland has been rising. In 2018, 1,136 alcohol-specific deaths were registered in Scotland2
Learning Bite
Alcohol related deaths are increasing in Scotland.
Definition
Alcoholic liver disease (ALD) is a clinical and histological spectrum of disease, which includes fatty liver (FL) at one extreme and alcoholic cirrhosis (AC) at the other.
FL is generally benign and asymptomatic and occurs in patients who abuse alcohol for a period of days to weeks. It is entirely reversible with abstinence from alcohol. With susceptibility and continued alcohol abuse more advanced disease can develop with alcoholic hepatitis (AH), an inflammation of the liver, which can lead to or exist with, AC in which the liver can become fibrosed.
Learning Bite
Alcoholic liver disease can be thought of as a spectrum from reversible fatty liver to alcoholic hepatitis to alcoholic cirrhosis.
Basic Science and Pathophysiology
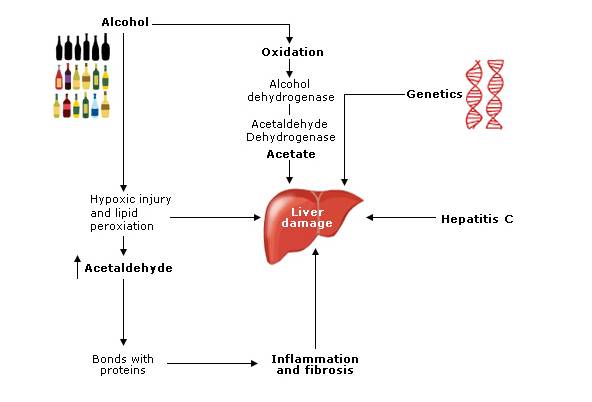
The development of ALD is mulitfactorial including female sex, viral hepatitis, genetics, age and induction of liver enzymes by other drugs.5 There are various mechanisms by which it is believed the liver becomes damaged by alcohol.
1. Acetate – Altered Carbohydrate Metabolism
The metabolism of ethanol (alcohol) occurs in the mitochondria where it is oxidised to alcohol dehydrogenase. This is then oxidised to acetate by acetaldehyde dehydrogenase. These reactions alter the redox state of the cell and can have detrimental effects on lipid and carbohydrate delivery, metabolism and export from the liver causing triglyceride accumulation (fatty liver).1,5
2. Acetaldehyde – Direct Hepatocyte Damage
Acetaldehyde concentration is increased in the liver with sustained alcohol intake resulting in hepatocytes becoming susceptible to hypoxia and hypoxic injury. Oxygen free radicals caused injury to hepatocytes by lipid peroxidation.1
3. Inflammatory Response
Acetaldehyde forms covalent bonds with proteins, which are antigenic. Long-term exposure to alcohol causes the body to amass circulating antibodies to these proteins resulting in harmful humeral and cellular responses.
In alcoholic liver injury the expression of pro-inflammatory cytokines is up regulated resulting in fibrosis.1 Collagen is deposited in the space of disse, which progresses to fibrosis and cell linkage formation resulting in cirrhosis. Lesions occur in the hepatic veins causing thickened veins and perisinusoidal fibrosis5 which can lead to cirrhosis.
4. Genetics
Genetic factors have been implicated by studies which have found a relationship between ALD and polymorphisms of alcohol metabolising enzyme systems (ALDH2, Cytochrome p450) and cytokines (TNF, IL1, IL10).3
5. Hepatitis C
Hepatitis C infection and alcohol have an additive effect together. This is thought to occur as alcohol may alter the immune systems efforts at clearing the virus or it may be due to increased iron deposition in liver secondary to high levels of alcohol, which can alter the pathophysiology of the virus.1
Hepatitis C and ALD also increases the chance of developing hepatocellular carcinoma significantly.5
Learning Bite
Development of ALD is mutifactorial and includes sex, hepatitis infections, and genetics.
Clinical Features
Such liver damage can be potentially life-threatening:
- Alcoholic hepatitis (AH) can result from prolonged alcohol abuse and presents with non-specific systemic symptoms; and can also cause features of portal hypertension.
- Alcoholic cirrhosis (AC) results in severe liver injury and shrinkage with increased portal hypertension and associated complications as well as decline of liver synthetic function.4
It is important to remember that alcohol can cause significant damage to the liver and health in general without producing any physical signs or symptoms. A vast majority of patients are diagnosed on routine blood tests.
Symptoms
Early symptoms may be non-specific and thus can require a certain clinical acumen to diagnose. More advanced disease may present with typical signs of liver disease. Sequelae of alcohol abuse may also be the presenting complaint, such as injuries.1
Clinical History
An open mind is required for all patients, especially within the ED, and alcohol intake should be part of every clinical history, although patients may be unaware that their intake is high or may deny the problem.
Collateral history is often important in these situations.
The Spectrum of Alcoholic Liver Disease
Symptomatic
The majority of cases of early liver damage can be diagnosed incidentally on routine blood tests in the ED or primary care. Many patients with fatty liver will be asymptomatic, hepatomegaly on examination may be the only finding.
Early symptoms of alcoholic liver disease
The majority of early symptoms of sustained alcohol abuse are generally non-specific symptoms, such as abdominal discomfort, vomiting or anxiety.
Injuries associated with intoxication
Often the first attendance to the ED of patient with potential ALD is due to a consequence of alcohol, such as falls, rib fractures, head injury or domestic violence.
Alcoholic hepatitis
These patients will often look more unwell with pyrexia and anorexia. Their liver function tests will be deranged and they may have clinical signs of chronic liver damage.
Portal hypertension
Clinical findings in portal hypertension are caused by blood being forced down different channels as the portal system pressure rises due to liver damage. Signs include ascites, varices (rectal and oesophageal), dilated abdominal veins, caput medusa with the risk of developing encephalopathy.
Cirrhosis
This is the end point of liver damage and is when the liver tissue is replaced by scar tissue due to the sustained damage caused by alcohol.
The synthetic function of the liver is compromised leading to bleeding and metabolic complications together with complications of portal hypertension mentioned previously.
Screening Tools
A number of screening tools can be used in the ED and they are as follows:
The CAGE questionnaire:
C. Have you ever felt the need to cut down you drinking?
A. Have you ever felt annoyed by criticism of your drinking?
G. Have you ever felt guilty about your drinking?
E. Have you ever taken a drink (eye opener) first think in the morning?
Similarly the FAST (Fast alcohol screening tool) questions are useful for ED settings. This is a concise version of the AUDIT screening tool5,7
The Paddington Alcohol Test (PAT) has also been shown to be a quick and easy method to identify hazardous drinkers in the ED.8
Learning Bite
Screening questionnaire tools should be used to identify problem drinking in the Emergency Department.
Management in the ED
The essential component of management in the ED includes recognising problem drinkers by including alcohol history in all assessments, especially in alcohol related injuries and suspected ALD.
A brief 10 minute opportunistic advice conversation with those found to have hazardous drinking (5 units per day for men or 3 units per day for women) has been found to be beneficial in raising awareness and reducing alcohol intake before it becomes harmful.9,10
Learning Bite
Brief interventions in the ED are effective in reducing alcohol intake.
Symptoms and Signs
Patients with FL are usually well. Hepatomegaly on examination may be the only sign of liver disease found.1
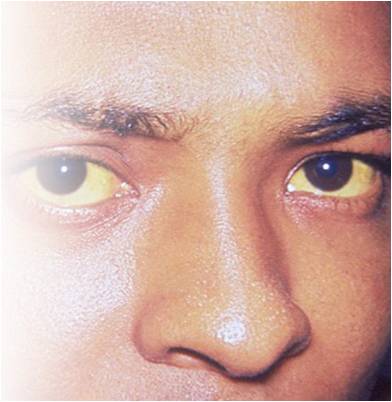
Patients suffering from AH often look unwell with pyrexia. They can be jaundiced and show cutaneous signs of chronic liver damage. Tender hepatomegaly is found on palpation. Ascites and encephalopathy can develop but varices are rare although bleeding may arise from gastric erosions exacerbated by coagulopathy.1
Features of AC include spider naevi, enlarged parotid glands, gynaecomastia, ascites, splenomegaly, palmer erythema, peripheral neuropathy, testicular atrophy.1,5 Portal blood flow together with hepatic vascular resistance are both increased secondary to alcohol consumption this increases portal pressure and collateral blood flow thus increasing the risk of variceal bleeding in patients with alcoholic cirrhosis and increased portal hypertension.1
Learning Bite
Clinical signs of liver disease may be subtle even with significant pathology.
Risk Stratification
One unit of alcohol is equivalent to 8g of ethanol (half pint of beer 3.5% or 25ml of spirits). Hazardous drinking is defined as regular daily consumption of over five units of alcohol for men (>40g) and over three units for women (>24g). Harmful drinking causes damage to physical or mental health.
Alcohol dependence is behaviour centred on the need to drink alcohol.9
Evidence suggests drinking 60-80g per day of alcohol for men and >20g per day for women increases the risk of ALD. Although studies have shown a low number 13.5% of patients with alcohol intake >120g per day developed ALD.
Risk Factors
Clearly there are risk factors which increase the likelihood of this happening, such as:
- Age
- Gender
- Genetics
Alcoholic cirrhosis occurs in only 8-20% of alcoholic patients and AH in 6-30%.
The prognosis (long-term) improves with abstinence; the five year survival rate for those with compensated cirrhosis who continue to abuse alcohol is less than 70% with survival of >90% if they stop drinking. Decompensated liver disease survival drops to 30% in five years for those still drinking alcohol.4
Learning Bite
Prognosis in all stages of ALD improves with abstinence from alcohol.
Biomechanical Tests
Serum biochemical tests are useful for the diagnosis of alcoholic liver disease:
Aspartate aminotransferase and alanine aminotransferase
Aspartate aminotransferase (AST)/alanine aminotransferase (ALT) ratio >2 differentiates between ALD and other liver pathology. Impaired ALT rise results from a hepatic deficiency of pyridoxal-6-phosphate required for ALT enzyme activity in the liver.5
Gamma-glutamyltransferase
Gamma-glutamyltransferase (GGT) is often found to be raised. These markers assess alcohol abuse indirectly by testing liver damage and therefore have a low sensitivity and specificity of less than 70%.
Mean corpuscular volume
Mean corpuscular volume (MCV) is also found to be raised in most cases due to toxic effects of alcohol on bone marrow. This marker also has low sensitivity in the region of 50%.
Prolongation of the prothrombin time
Prolongation of the prothrombin time (PT) and low albumin levels suggest poor synthetic liver function.5
The emerging tests below are sometimes used in conjunction with above tests:
Carbohydrate-deficient transferrin test
Carbohydrate-deficient transferrin test shows the desialylation of transferrin which occurs in the presence of high alcohol intake independent of liver damage. This is thought to be specific for ALD, although it has relatively low sensitivity.
Mitochondrial aminotransferase
Mitochondrial aminotransferase (AFT) is released from hepatocytes with sustained alcohol abuse.
Diagnosis
Ratio of AST/ALT 1.5:2
Low albumin
High PT
High MCV
Low platelets
Other Tests
Ultrasound may be helpful to investigate liver damage. Fatty liver and alcoholic hepatitis are demonstrated by changes in liver parenchymal reflectivity. A cirrhotic liver is irregular and shrunken. Doppler studies may show slow or reversed portal vein flow, which, together with splenomegaly and intra-abdominal varices, would indicate portal hypertension.1,5
Liver biopsy can be useful to confirm diagnosis such as AH prior to treatment. With ALD and viral hepatitis, prognostic and management information can be gained from studying the necroinflammatory changes at biopsy.5
The coagulopathy associated with liver disease increases the risk of complications and therefore the transjugular venous route is sometimes preferred.1
Learning Bite
The majority of patients are diagnosed with ALD on routine blood tests.
Thiamine Deficiency
Thiamine deficiency can cause a neuropsychiatric complication (Wernicke’s encephalopathy), which often occurs in chronic alcohol users and particularly during withdrawal. It is characterised by confusion, ataxia, hypothermia, hypotension, nystagmus and vomiting.
The classic triad of confusion, ataxia and ophthalmoplegia is only present in approximately 10% of patients with this condition and therefore a high index of suspicion is required. If untreated this condition can progress to Korsakoffs psychosis. The severe short-term memory loss and functional impairment, which this condition results in, renders the patient to require permanent institutionalised care.6
Thiamine administration
Thiamine should be administered to patients prior to a glucose load to prevent the diminished thiamine stores becoming exhausted and triggering Wernickes onset.1
Oral thiamine is poorly absorbed in dependent drinkers and so parenteral thiamine may be considered in all patients and definitely if any features of Wernickes encephalopathy are present.11 Oral thiamine should be given in divided doses to maximise absorption (300 mg per day).9
Learning Bite
Thiamine should be given to all ALD patients who come to the ED.
Investigation
Patients should be investigated appropriately in the ED using blood tests and imaging as available. ED doctors should act on abnormal blood results and seek help from specialists. Appropriate patients should then be referred to GI for ongoing management. Patients displaying evidence of advanced or acute disease should be admitted under the gastrointestinal (GI) physicians for specific management.
Most patients who are withdrawing from alcohol can be managed at home with no drugs or small doses of benzodiazepines for withdrawal. Patients at high risk of complicated withdrawal may benefit from a short inpatient stay to monitor them and adjust their drug doses as appropriate.
Observational studies have shown a strong correlation between involvement in Alcoholics Anonymous and long-term abstinence6. If patients present to the ED requesting detoxification they should be advised to make an appointment with their GP and be given contact information for community support organisations.
Management of Alcoholic Liver Disease
The essential part of successful management of ALD is abstinence from alcohol. Fatty liver can be entirely reversible and other later presentations can be stabilised and improved with cessation of alcohol. Continuing to drink is the best predictive indication of a poor outcome.5
Diet
Specific attention to diet has shown to be beneficial in ALD patients. Malnutrition in ALD patients should be improved with a high protein diet (25-35 kcal/kg of ideal body weight).
Studies have shown patients who had at least 2500 kcal per day had improvements in liver function and six month survival than those who had less. Enteral feeding maximises digestion and may improve long-term survival in ALD patients.
Interestingly, although obesity can be an independent risk factor for ALD progression, weight loss has not been shown to be of benefit in alcoholic fatty liver disease and may actually worsen liver injury.5
Learning Bite
At all stages of ALD, abstinence is key to management.
Ongoing Management
Complications of portal hypertension
As with other types of liver disease, complications of portal hypertension should be considered and managed appropriately, such as:
- Encephalopathy
- Oesophageal varices
- Ascites and liver synthetic function derangement
- Hypoglycaemia
- Coagulopathy
Caution should be taken when diagnosing encephalopathy in this patient group as the differentials include subdural haematoma, Wernickes encephalopathy and delirium tremens.1
Liver transplantation is the only curative treatment for advanced ALD, however current or recent substance abuse is a contraindication for transplant. Selection requires a multi-disciplinary team approach including a hepatologist, surgeon, addiction specialist, psychiatrist and social worker. Patients must be motivated and compliant with immunosuppressive treatment.4
Relapse of alcoholism after transplant is sadly common, the best predictor for continued sobriety after transplantation is a period of 6 months or longer documented abstinence.1,5
Alcohol interferes with compliance and metabolism of immunosuppressive medications and recipients who succumb to alcoholism often rapidly develop liver damage in the graft including cirrhosis.1,4
Learning Bite
Liver transplant is the only hope for cure in advanced ALD.
- Failing to question patients about alcohol intake when they present to the ED
- Not acting on abnormal blood results on asymptomatic patients
- Failing to refer patients to alcohol support services or a GI specialist when appropriate
- Failing to give thiamine to a patient suspected of alcoholism
- Not recognising more serious aspects such as development of Wernickes encephalopathy or pathology secondary to alcohol related injuries, such as a subdural haematoma
- Alcohol related deaths are increasing in Scotland
- Alcoholic liver disease can be thought of as a spectrum from reversible fatty liver, to alcoholic hepatitis, to alcoholic cirrhosis
- Development of alcoholic liver disease is multifactorial, including sex, viral infections and genetics
- The majority of patients are diagnosed with alcoholic liver disease on routine blood tests
- At all stages of alcoholic liver disease, abstinence is key to management [Evidence grade: 4, grade of recommendation: C]
- Ongoing heavy alcohol intake is the best predictor of a poor outcome in early alcoholic liver disease
- Thiamine should be given to all alcoholic liver disease patients who come to the emergency department [Evidence grade: 2b, grade of recommendation: B]
- Liver transplant is the only curative treatment for advanced cirrhosis [Evidence grade: 4, grade of recommendation: C]
- Walsh D, Alexander G. Alcoholic liver disease. Postgrad Med J 2000;76:280-286. View abstract. [Last accessed Feb 2020].
- NHS Alcohol Information Service. Alcohol Statistics Scotland 2019. View website. [Last accessed Feb 2020].
- Reuben, A. Alcohol and the liver. Current Opinion in Gastroenterology 2006; 22: 263-71
- Menon NKV, Gores AJ, Shah VH. Pathogenesis, diagnosis and treatment of alcoholic liver disease. Mayo Clin Prac 2001;76:1021-1029. View abstract. [Last accessed Feb 2020].
- Mendez-Sanchez N, Almeda-Veldes P, Uribe M. Alcoholic liver disease: An update. Annals of hepatology 2005;4:32-42.
- Parker AJR, Marshall EJ, Ball DM. Diagnosis and management of alcohol use disorders. BMJ 2008;336:496-501. View abstract. [Last accessed Feb 2020].
- Imperiale TF, McCullough AJ. Do corticosteroids reduce mortality from alcoholic hepatitis? A meta-analysis of the randomised trials. Ann Intern Med 1990;113:299-307. View abstract. [Last accessed Feb 2020].
- Smith SG, Touquet R, Wright S et al. Detection of alcohol misusing patients in accident and emergency departments: the paddington alcohol test (PAT). J Accid Emerg Med 1996;13:308312. View abstract. [Last accessed Feb 2020].
- NICE. Alcohol-use disorders: diagnosis, assessment and management of harmful drinking (high-risk drinking) and alcohol dependence. View here. [Last accessed Feb 2020].
- Best BETs. Brief intervention for adults attending the emergency department due to alcohol. View article. [Last accessed Feb 2020].
- Best BETs. Who requires prophylactic vitamin B supplementation. View article. [Last accessed Feb 2020].