Author: Paul A Younge / Editor: Jason Kendall / Reviewers: Mohamed Elwakil, Stewart McMorran, Emma Everitt / Codes: A1 / Published: 27/01/2020
Definition of bradycardia
Bradycardia is defined as a heart rate of less than 60 beats per minute.
The causes of bradycardia can be broadly categorised as follows: normal physiological variants, intrinsic cardiac problems, or secondary to infections, drugs, autonomically-mediated causes and systemic illness (eg. metabolic and endocrine derangement). See Box 1.
Primary cardiac aetiologies are the result of congenital or acquired structural problems, ischaemia, infarction, infection or fibrosis directly affecting the sino-atrial (SA) node, atrioventricular (AV) node or His-Purkinje system.
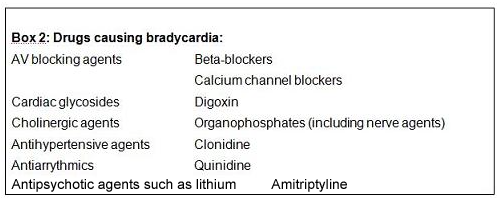
Various drugs can also affect the electrophysiology of the heart myocytes and their nerve supply (see Box 2).
Bradycardia may present as an incidental finding or with symptoms related to hypotension (see Box 3). Other symptoms may relate to the underlying cause.
The different types of bradycardia are classified in Box 4:
The causes, clinical presentations and management for each type of bradycardia are discussed in more detail in the sections below. A final section describes drug therapy and pacing in more detail.
Basic science and anatomy
Figure 1: The conduction pathways of the heart.

The conduction pathways of the heart consist of:
- The sinoatrial node
- The Atrioventricular node
- The Bundle of His
- The left and right bundles
- The Purkinje fibres
Signals arising from the SA node stimulate the atria to contract and are conducted to the AV node (the P wave on the ECG). Normally electrical activity is spontaneously generated by the SA node (the physiological pacemaker ). The impulse is propagated from the right atrium to the left atrium via Bachmanns bundle. Conduction to the AV node occurs in specialised tissue called intermodal tracts. The AV node introduces a critical delay (the PR interval) into the conduction system allowing blood to flow from the atria into the ventricles. The distal part of the AV node is called the Bundle of His which splits into two bundle branches in the interventricular septum (left and right). The left bundle branch activates the left ventricle, whilst the right bundle activates the right ventricle. The left bundle splits further into the left anterior fascicle and left posterior fascicle. The two bundle branches taper out to produce numerous Purkinje fibres which stimulate individual groups of myocardial cells to contract. The spread of electrical activity through the ventricular myocardium produces the QRS complex on the ECG.
Disruption to parts of this conduction system will result in failure to generate impulses (eg. sick sinus syndrome, sinus arrest) or in failure to propagate impulses at various levels of the system (eg. AV nodal block, complete heart block, etc.).
General approach and principles of management
The urgency of management depends on the degree of haemodynamic compromise or shock present. Management will also be determined by the specific cause of, and site of, the conduction disturbance.
Learning Bite
The urgency of treatment of bradycardia depends on the degree of haemodynamic compromise.
However certain general principles or management steps pertain to all cases and are listed in Box 5:
The following sections describe the various types of bradycardia and their specific treatment points in more detail.
Sinus Bradycardia
In sinus bradycardia the heart rate is below 60 bpm and there is a P wave before every QRS complex. The PR interval is constant. Causes are listed in Box 1.
Clinical features:
Sinus bradycardia may be normal in healthy young adults, especially athletes.
It may also be normal in those taking an appropriate dose of beta-blockers. In these cases patients will be asymptomatic.
It is considered pathological if it results in decreased cardiac output causing any or a combination of the symptoms in Box 3.
Management:
In the absence of hypoxia and/or shock, the first line treatment for all symptomatic bradycardias that are unlikely to resolve spontaneously and expeditiously (e.g. in the setting of posterior or inferior MI or vagal syncope) is intravenous atropine 0.5 mg initially. Consideration must also be given to the underlying cause.
Some specific causes of sinus bradycardia:
(i) Hypothermia:
A specific cause of sinus bradycardia which must not be overlooked in the elderly is hypothermia. The ECG may contain J waves (see Figure). J waves occur immediately after the QRS complex; their size may be proportional to the degree of hypothermia and they resolve with successful rewarming.
Figure: ECG of a hypothermic patient demonstrating J waves
(ii) Drugs:
Deliberate or iatrogenic drug overdose with AV nodal blocking agents, digoxin, organophosphates and other agents may require pharmacological treatment in addition to pacing. Individual drugs may cause other symptoms and signs (see below and the relevant toxicology sessions).
Beta Blockers:
Atropine is unlikely to work. Beta agonists such as adrenaline and isoprenaline are effective as infusions. Adrenaline is preferred due to its short half-life. There is anecdotal evidence for the use of high dose intravenous glucagon.
Calcium channel antagonists:
Again atropine is unlikely to be effective. Intravenous fluid loading and intravenous calcium are the mainstays of treatment followed by an adrenaline infusion if required.
Digoxin:
Normally causes a slowing of pre-existing atrial fibrillation. Occasionally a regularisation of the rhythm occurs (similar to a nodal bradycardia). Toxicity is worsened by hypokalemia which should be corrected if present. In severe cases an antidote is available (Fab fragments of digoxin antibodies).
Organophosphates:
Bradycardia is part of a cholinergic syndrome. Large doses of Atropine are required titrated to a point when the patients mouth is dry.
(iii) Head injury:
Significant head injury with raised intracranial pressure is associated with sinus bradycardia and raised blood pressure (Cushings Response); it is an ominous sign and is caused by brain stem compression.
Learning Bite
Bradycardia and hypertension in a patient with a head injury is an ominous sign and is associated with significantly raised intracranial pressure.
Sinus Arrest
Often intermittent and interspersed with a normal rhythm, sinus arrest is characterised by the absence of P waves and pauses of 3 seconds or more (see Figure). It is the result of either sinus node disease or carotid sinus hypersensitivity.
Figure: Prolonged sinus arrest associated with carotid hypersensitivity.
Clinical features:
It can be asymptomatic and a coincidental finding or cause pre-syncope.
Various syndromes such as cough or micturition syncope are thought to be the result of carotid sinus hypersensitivity. Vasovagal episodes may also be related to periods of sinus arrest.
Management:
Exacerbating drugs such as beta blockers or calcium channel antagonists should be stopped. Rarely a permanent pacemaker is required.
Sinus node disease (sick sinus syndrome)
Sinus node disease can present with sinus bradycardia (see above), sinus pauses or sinus arrest (see above) or tachycardia-bradycardia (tachy-brady ) syndrome where patients have episodes of both bradycardia and tachycardia. Other ECG characteristics of sick sinus syndrome may include a varying p wave configuration and an irregular heart rate in the presence of p waves with a relatively constant PR interval.
The pathophysiology is usually acute or chronic cardiac ischaemia, dilated cardiomyopathy or age related fibrosis of the SA node. It has a poor prognosis with 5 year survival rates in the range of 47-69%.
Learning Bite
Sick sinus syndrome can present with sinus bradycardia, sinus pauses, or with a tachycardia-bradycardia syndrome.
Figure: Rhythm strip from a patient with sick sinus syndrome showing significant sinus pauses
Management:
It may respond to oxygen and judicious intravenous fluids with treatment of cardiac ischaemia (reperfusion therapy) where appropriate. Atropine has a variable effect. Temporary then permanent trans-venous pacing is usually required often combined with drugs to prevent tachycardias (e.g. sotalol).
Junctional Bradycardia
A junctional bradycardia is a regular rhythm initiated in the AV nodal tissue and occurs when the SA nodal pacemaker fails. This escape rhythm is characteristically 40-60 bpm and has a narrow complex (see Figure).
It is not usually a physiological response; causes of junctional bradycardias are listed in Box 1. It can occur during cardiac reperfusion.
Clinical features:
It may present as a coincidental finding or with symptoms related to the bradycardia as listed in Box 3.
Management:
Treatment is required if there is haemodynamic compromise: identify causative factors and correct if possible. First line pharmacological treatment is intravenous atropine (0.5 mg)
Prognosis is usually good but in persistent cases permanent pacing may be required.
Figure: High junctional bradycardia in the setting of an acute coronary syndrome
Atrioventricular block
AV block occurs when atrial depolarisation fails to reach the ventricles because of a block involving the AV node or the His-Purkinje system.
If block is at the AV nodal level complexes will be narrow. If block is lower down in the His-Purkinje system complexes will be wide. The higher the block the more likely it will respond to increases in sympathetic tone or the use of atropine.
Three degrees of block are recognised and described below:
(i) First degree AV block:
Conduction is delayed within the AV node resulting in a constant prolongation of the PR interval on the ECG (which is defined as being greater than 200 milliseconds) and the QRS complex remains narrow.
This may be a sign of early fibrosis or ischaemia in the AV node but is most commonly a normal variant and is asymptomatic. In the context of an acute coronary syndrome it requires monitoring in case of progression to other forms of heart block. It does not require treatment.
(ii) Second degree AV block:
The QRS remains narrow but atrial impulses fail to conduct normally to the ventricles in one of the following ways:
Mobitz type I (Wenckebach)
The PR interval lengthens progressively after each successive P wave until a P wave is not conducted (see Figure). This is common following inferior acute myocardial infarction (AMI) when it may progress to complete heart block. It is normally asymptomatic and requires monitoring but not urgent intervention.
Learning Bite
Mobitz type 1 heart block (Wenckebach) is normally asymptomatic and resolves without the need for urgent intervention.
Figure: 2nd degree heart block, Mobitz Type 1 (Wenckebach)
Mobitz type II
There is a constant PR interval but some P waves fail to conduct to the ventricles (see Figure). The ratio of conducted and non-conducted beats may be fixed (e.g. 2:1 or 3:1). This is less common than Mobitz type I, often symptomatic and of more concern. It signifies septal involvement in the setting of AMI and commonly progresses to complete heart block. Patients who have this diagnosed on pre-operative assessment are fitted with pacemakers before undergoing anaesthesia.
Figure: Second degree heart block, Mobitz Type 2 (2:1 block)
Learning Bite
Mobitz type 2 heart block commonly progresses to complete heart block which may require urgent intervention.
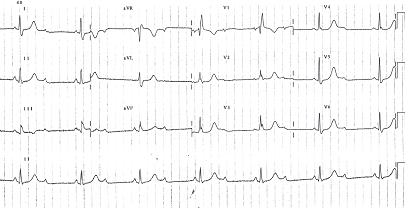
(iii) Third degree AV block (Complete heart block):
All P waves fail to conduct to the ventricles resulting in a broad complex ventricular escape rhythm (see Figure). A rhythm originating in the high septal region will have a rate of 40-50 beats per minute. If originating from a lower ventricular site the rate will be lower at 30-40 beats per minute. Although this may be a coincidental finding it usually presents with lethargy and syncope. It signifies significant fibrosis or ischaemia in the AV node and requires a permanent pacemaker. Following an anterior AMI it indicates extensive damage to the septal region and indicates a worse prognosis.
Figure: Third degree AV block (Complete heart block)
Learning Bite
Complete heart block in the setting of acute anterior MI indicates extensive septal damage and is a poor prognostic sign.
Specific interventions for Bradycardias
(i) Atropine
Although this is the first line treatment for symptomatic bradycardia, atropine will not always be effective. It competitively blocks the action of acetylcholine at muscarinic receptors thus blocking the action of the vagus nerve on the SA and AV nodes. High vagal tone is prominent in autonomic mediated bradycardia and may be a contributing factor in systemic illness and acute coronary syndromes. Atropine is very effective in the presence of high vagal tone but may have little effect on a fibrosed AV node or in most cases of drug toxicity (except organophosphates). In atropine resistant cases pacing and/or vasopressors may be required.
Atropine is effective in Mobitz type I heart block and third degree blocks with high nodal escape rhythms. It is less effective in bradycardias due to drug toxicity (except organophosphates), Mobitz type II block and third degree block with a low Purkinje or ventricular escape rhythm.
At doses below 0.5 mg it may paradoxically worsen bradycardia. A dose of 3 mg is thought to completely block the vagus nerve.
It must be remembered that atropine is not a short acting drug and has an elimination half life of 2 to 3 hours, thus side effects such as a dry mouth, blurred vision and resting tachycardia will be prolonged. Its use should be carefully considered, therefore, in self limiting situations such as transient brady-arrhythmias related to inferior AMI.
Learning Bite
Atropine at a dose of 0.5mg is the first line treatment for most symptomatic bradycardias.
(ii) Inotropes
Following correction of hypoxia, hypovolaemia and ischaemia, atropine or temporary pacing may still be ineffective in treating bradycardia and/or its associated hypotension. In these cases it may be necessary to use an inotrope. The main choices are between isoprenaline and adrenaline.
Isoprenaline:
This acts mainly on beta-1 receptors and thus acts mainly as a positive chronotrope. It has a 60 to 90 minute duration of action. Because of its relatively long half life and the consequent difficulties in titration for optimum effect it has fallen out of favour for this situation. It also reduces systemic vascular resistance so may exacerbate hypotension especially in the presence of other vasodilator drugs such as calcium channel blockers.
The usual starting dose is 5 mcg/min.
Adrenaline:
This is a non-selective adrenoreceptor agonist acting on beta and alpha receptors. It is potent and has a very rapid onset and offset (less than one minute). It is now the preferred inotrope for this indication. Infusions lasting more than a few hours can result in gut ischaemia and metabolic acidosis. Thus it should be seen as a temporising measure before transvenous pacing.
The usual starting dose is 2-10 mcg/min
(iii) Pacing
Initial pacing, particularly if required urgently, is usually non-invasive and takes the form of percussion or transcutaneous pacing (see below). These are the most common pacing interventions used in the ED. Typical indications are listed in Box 5
Transvenous pacing is usually indicated if percussion or transcutaneous pacing have been employed as a temporising measure and are commonly performed in in-patient settings (radiological screening is required) as is the placement of permanent implanted pacemakers.

Percussion pacing:
This is most appropriate in the setting of ventricular standstill where there is evidence of P wave activity, used as an alternative to CPR. It can also be used for other bradycardias with haemodynamic compromise whilst attaching transcutaneous pacing pads.
It is performed by delivering firm blows over the precordium lateral to the left sternal edge. Position and firmness of blows can be adjusted to achieve capture and an appropriate threshold.
Transcutaneous pacing:
Pacing pads can be rapidly applied and operated easily by medical and paramedical staff. This form of pacing can cause the patient discomfort due to chest wall muscle contraction. Pads are applied to the right sternal edge and apex (or in anterior-posterior positions). The pacing module is set on demand mode, an appropriate rate set and the pacing current increased until capture is achieved (a QRS complex following each pacing spike).
Key Learning Points
- Bradycardia is defined as a heart rate of less than 60 beats per minute
- The urgency of treatment of bradycardia depends on the degree of haemodynamic compromise
- Use atropine 0.5 mg intravenously as first line drug in most cases of symptomatic bradycardia
- Establish transcutaneous pacing if bradycardia causing haemodynamic compromise and atropine ineffective
- Start inotropes if above measures are ineffective or there is ongoing hypotension
- Sick sinus syndrome can present with sinus bradycardia, sinus pauses, or with a tachycardia-bradycardia syndrome
- Mobitz type 1 heart block (Wenckebach) is common following inferior acute myocardial infarction (AMI); it is normally asymptomatic and requires monitoring but not urgent intervention
- Mobitz type 2 heart block is often symptomatic and of concern. It signifies septal involvement in the setting of AMI and commonly progresses to complete heart block
- Complete heart block in the setting of acute anterior MI indicates extensive septal damage and is a poor prognostic sign
- Resuscitation Council (UK). Adult Advanced Life Support Guidelines 2015.
- Ghuran A, Uren N, Nolan, J. Emergency Cardiology, an Evidence Based Guide to Acute Cardiac Problems. Arnold, London 2003. ISBN 0340807199.
- Myerson S, Choudhury R, Mitchell A. Emergencies in Cardiology. Oxford University Press 2005. ISBN 9780856959.
- Livingstone M, Overton D. Sinus Bradycardia. E Medicine 2009.
- Laurence L. Brunton ed. Goodman & Gilmans The Pharmacological Basis of Therapeutics 11e. Mcgraw Hill 2009.
- Boyd R. Glucagon for the treatment of symptomatic B-blocker overdose. Best BETs 2003.